A Pelvic Floor Therapist’s Perspective to Lumbopelvic Pain
To anyone who has experienced it first hand, it’s no secret that the economic, physical, and socio-emotional burden of back pain is enormous. However, did you know that despite the range of available therapeutic interventions, about 80% of Americans will experience back pain at some point in their lives. This huge percentage indicates some serious shortcomings in current approaches.
Lower back pain (LBP) is in the top 3 reasons for visiting a primary healthcare provider. Back pain is one of the leading causes of job-related disability and a major contributor to missed workdays. The combination of lower back and hip pain, or an umbrella term called lumbopelvic pain, is only on the rise. From 1990-2013, there was a 57% increase in the global prevalence of lumbopelvic pain, and these numbers are expected to continue to increase as the population ages.
The causes of lumbopelvic pain is multifactorial, spanning from mechanical, psychological, and social factors. In the last 10 years there have been increasing research analyzing the relationship between lumbopelvic pain and pelvic floor muscle dysfunction.
Pelvic floor muscle dysfunction refers to an array of manifestations related the pelvic floor musculature: urinary incontinence, sexual dysfunction, pelvic pain, and pelvic organ prolapse. Regardless of the functional impairment, pelvic floor dysfunction is examined through testing the range of motion, strength, coordination, resting muscle tension of the pelvic floor muscles, as well as sensory-motor processing regulation.
1 in 5 women experience urinary incontinence
50% of women over the age of 40 have a pelvic organ prolapse
Dyspareunia (painful intercourse) in the United States is approximately 10% to 20% of women
Despite the high volumes of scientific literature, overall protocol and treatment practices have remained the same. The link between the pelvic floor and lumbopelvic pain is becoming evident, especially with women.
95% of people who report lower back pain also have pelvic floor muscle dysfunction (Dufour, et al, 2018).
A recent study (Keizer et al, 2019) found that women with lumbopelvic pain and urge incontinence are 2.93 times more likely to have tenderness on palpation of the pelvic floor than those without urge incontinence. There appears to be a relationship between pelvic floor muscle tenderness and presentations of lumbopelvic pain with self-reported urinary urgency and central sensitization (perceptions of pain), both of which can be treated effectively by pelvic health therapists.
When it comes to lower back pain, it’s time to start seeing the bigger picture and realize that it’s all connected.
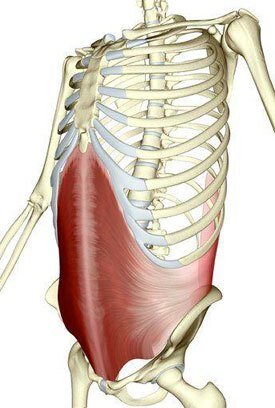
In this case, it’s actually physically connected, by the transverse abdominis (TA) and multifidus. The TA is the deepest abdominal layer and the multifidus is a postural muscle along the spine. These two muscles are part of the deep core system that work to support the spine and anticipate movement.
Multifidus Image Source: Balham Sports ClinicTransverse Abdominis Image Source: AlamyIf you’re not aware of the deep core system, I recommend you peruse through another cOre poTential post about the Diaphragm, Core, & Pelvic Floor.
TL:DR— the TA, multifidus, diaphragm, and pelvic floor work as a team. Yes, they are all connected.
I like to think about the TA as a corset because it covers the entire abdomen with origins points spanning from the rib cage, thoracolumbar fascia and the iliac crest, wrapping around to the inguinal ligament and pubic bone. It may be an abdominal muscle and serves to compress abdominal viscera and supports expiration, but it also connects to the posterior chain and aids in trunk rotation.
The multifidus plays a crucial role in lumbopelvic stability. A study from 2006 looked at lumbar multifidus atrophy following a lumbar root or disc injury. The findings showed that the multifidus atrophied within 24 hours of injury and never returned back to pre-injury size unless provided specific training. It also concluded that the likelihood of re-injury is high once there’s weakness.
...cough cough chronic back pain...The overlap of muscles and fascia in this area of the body further demonstrates the link between lower back pain and pelvic floor functioning.
Here’s the issue, the majority of physical and occupational therapists who are treating people with lumbopelvic pain are not trained to assess the pelvic floor. They end up missing a huge piece of the puzzle!
Dumoulin et al. suggested that the demand for care of pelvic floor musculature dysfunction will rise by 35% in the next 12 years. Realistically there’s no way to be the expert of all issues associated with lumbopelvic pain and pelvic floor muscle dysfunction. Improved multidisciplinary collaboration is a necessity, even just within the specialities of OT/PTs.
People who come to me have been down a long and frustrating path seeking help from physicians, physical therapists, chiropractors, and other health/wellness professionals with minimal long term success.
Are you someone who experiences lower back and hip pain?
Has regular treatment not helped to improve this pain?
You may be someone who could benefit from pelvic floor therapy. If you live in Boston or the Greater Boston area, Functional Wellness is here to help you heal from the inside out. Get back to the things you need, want, and love to do. It all starts with a free discovery call. Book your free call with the link below, and let’s talk.
Resources: Dufour S, Vandyken B, Forget MJ, Vandyken C. Association between lumbopelvic pain and pelvic floor dysfunction in women: a cross sectional study. Musculoskelet Sci Pract. 2018;34:47–53Dumoulin C, Hay-Smith EJ, Mac H-SG. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;5.Hodges P, Holm AK, Hansson T, Holm S. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine (Phila Pa 1976). 2006 Dec 1;31(25):2926-33. doi: 10.1097/01.brs.0000248453.51165.0b. PMID: 17139223.Keizer A, Vandyken B, Vandyken C, Yardley D, Macedo L, Kuspinar A, Fagahani N, Forget MJ, Dufour S. Predictors of Pelvic Floor Muscle Dysfunction Among Women With Lumbopelvic Pain. Phys Ther. 2019 Dec 16;99(12):1703-1711. doi: 10.1093/ptj/pzz124. PMID: 31504926.Contact Functional Wellness today!
Looking to book a session? Inquiries and more information?
Use the button below to schedule a free discovery call or initial evaluation, or write us a message using the form. We’ll respond within 24 hours, (likely sooner).